
Premature Retinopathy: Early Diagnosis is Crucial to Prevent Childhood Blindness
Premature Retinopathy (ROP) is an ocular condition that affects premature infants. According to retina disease and premature retinopathy specialist Samuel Montenegro, ROP is one of the primary causes of preventable childhood blindness. In Brazil, an estimated 13,500 cases occur annually, and among these cases, 1,000 infants may need treatment.
Therefore, identifying newborns in need of treatment early is crucial to reduce ROP-related blindness. Premature babies weighing up to 1.5 kilograms and/or born before 32 weeks’ gestation are a high risk group for ROP.
This period might extend to 35 weeks if the child experiences sepsis, intraventricular hemorrhage, respiratory distress syndrome, requires blood transfusions, or if the mother had a multiple pregnancy, even if the baby’s weight is above 1.5 kilograms.
This is because premature birth can disrupt the development of the baby’s retinal blood vessels. In these cases, vascularization might expand, twist, or even rupture. In advanced stages, this can lead to the formation of retinal scars or even retinal detachment, resulting in permanent vision loss.
The International Classification of ROP (ICROP) defines the disease by severity (stages 1-5), location (zones I-III), and extension in analog hours (1-12 h), with or without additional disease (arteriolar dilation and venous tortuosity), and the presence of which would indicate disease activity (4-5).
Check the table below:
| Premature Retinopathy Classification | |
| Stage 1 | White line separating vascular from avascular retina |
| Stage 2 | Elevated ridge |
| Stage 3 | Fibrovascular proliferation from ridge |
| Stage 4 | Proliferation leading to subtotal retinal detachment (4a, extrafoveal; 4b, total detachment, including fovea) |
| Stage 5 | Total retinal detachment (open or closed funnel) |
| Threshold disease (defined by CRYO-ROP) (untreated cases show poor anatomical outcomes in 50% of cases) | Stage 3 retinopathy, zone I or II, with at least five contiguous hours or eight cumulative hours of extension, with an additional disease disease (arteriolar dilation and venodilation). |
| Type 1 pre-threshold disease (defined by ET-ROP) | Any ROP in zone I with an additional disease (aggressive posterior disease) Stage 3, zone I, without plus disease Stage 2 or 3 in zone II, with additional disease(s). |
| Type 2 pre-threshold disease (defined by ET-ROP) | Stage 1 or 2, zone I, without additional disease(s) Stage 3, zone 2, without additional disease(s). |
Source: Proposed Brazilian guidelines for examination and treatment of retinopathy of prematurity (ROP).
Premature Retinopathy Assessment

ROP bears two dangerous characteristics: it’s silent, showing no visible symptoms, and it progresses rapidly. Therefore, adhering to international and national protocols for early diagnosis and treatment is crucial.
Montenegro explains that routine eye examinations for premature babies should be conducted four weeks after birth. “The child isn’t born with the disease, so it’s essential to assess during this period.”
The examination should be performed by an ophthalmologist experienced in evaluating preemies and knowledgeable about the disease to identify location and sequential retinal changes.
Subsequent examination scheduling will be determined by findings from the initial examination.
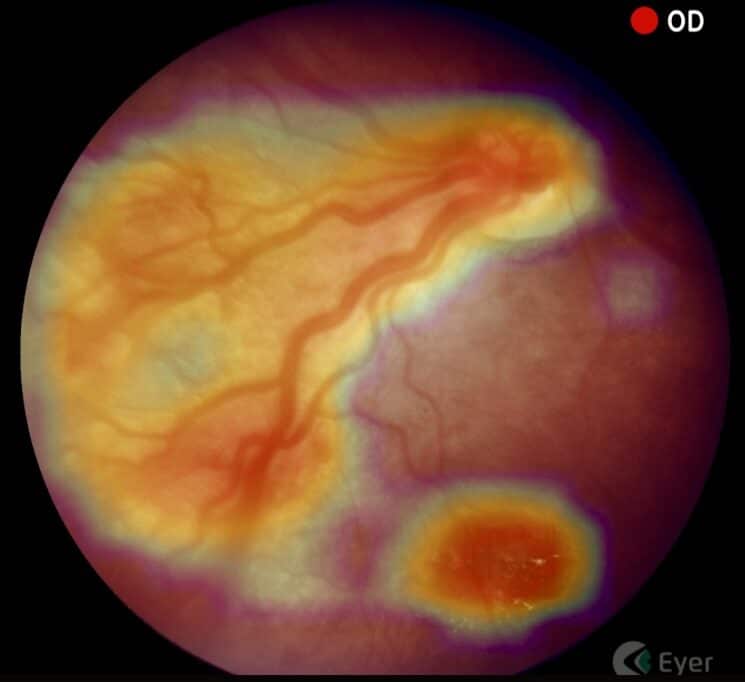
After identifying ROP, Montenegro tracks and documents patients using a portable retinal camera, Eyer. This equipment, highly recommended for infant and child examinations due to its portability and high image quality, attaches to a smartphone and conducts retinal exams within minutes. It also makes images available on the online platform, EyerCloud, facilitating study and case progression monitoring for physicians.

“The device has been a game-changer as it greatly assists me in capturing the patient’s retina at that exact moment, in a practical, quick, and high-quality manner,” he states. Previously, the specialist used a retina mapping lens with smartphone assistance for videos. “Then I’d freeze the image, take a screenshot, and store it on the computer. It was quite labor-intensive,” he recalls.
Premature Retinopathy Treatment
Montenegro explains that treatment is most effective when ROP is identified early. “The secret to managing this disease lies in early diagnosis and immediate treatment when necessary.”
Currently, retinal ablation with a laser is the gold-standard treatment. Depending on the stage, there are alternatives, such as anti-VEGF injections and cryotherapy. “In this disease, we’re fighting blindness. Therefore, we apply laser therapy to prevent blindness in cases where it’s the best indication. However, this may permanently restrict the field of vision,” he points out.
Children with ROP receive follow-up care from a multidisciplinary team: pediatric ophthalmologist, retina specialist, occupational therapist, and physiotherapist. This follow-up extends beyond retinal ablation, aiming to achieve early visual stimulation.
“Newborns diagnosed with ROP are at a higher risk of developing ophthalmological issues in the future, such as strabismus, amblyopia, and refractive errors. Therefore, ophthalmological follow-up after discharge is recommended,” he emphasizes.

ROP Brazil
Montenegro is part of a project called ROP Brazil, which aims to share knowledge and further study premature retinopathy.
Various surveys indicate that the proportion of blindness caused by ROP is greatly influenced by the level of neonatal care (availability of human resources, equipment, access, and quality of care), as well as the presence of effective screening and treatment programs. Consequently, there’s significant variability in disease occurrence between developed and developing countries.
“That’s why, understanding more about the disease is essential to decrease cases of preventable childhood blindness in the country,” he states.




